Summary
This invention uses new diagnostic procedures and probiotic treatment to improve the health and quality of life for patients with spinal cord injuries.
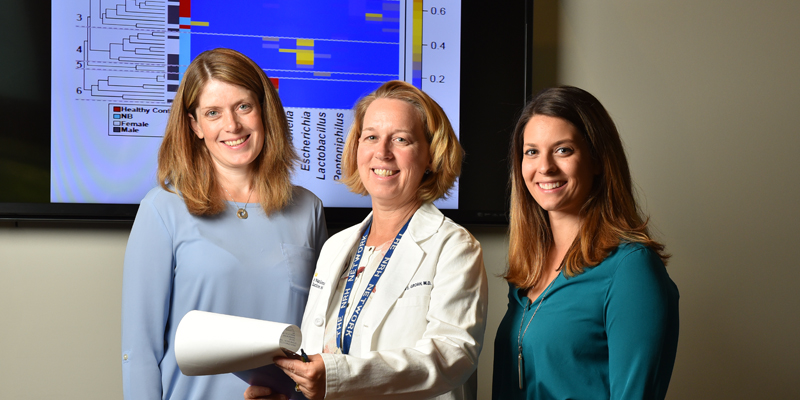
Inventors
What is it? What does it do?
Patients living with a Spinal Cord Injury (SCI) may suffer from common secondary complications with Neurogenic Lower Urinary Tract Dysfunction (NLUTD). NLUTD is defined as the loss of sensation and voluntary control of the bladder, commonly resulting from a variety of neurological conditions, including spinal cord injury and disease, spina bifida, Parkinson’s disease, stroke, multiple sclerosis, traumatic brain injury, and dementia.1
As a result, many SCI patients live with recurring Urinary Tract Infections (UTIs), causing decreased quality of life. A staggering one third of office and emergency department visits among people with NLUTD eventually lead to hospitalization annually, especially when septicemia, also known as sepsis, occurs in extreme cases.2,3,4
Dr. Suzanne Groah has invented a method for screening, diagnosing, and treating UTI in patients with spinal cord injuries who suffer from NLUTD, in partnership with her colleagues from the Spinal Cord Injury Clinical Programs and Research team at MedStar National Rehabilitation Hospital.
Why is it better?
-
This treatment method comes after the team’s research has shifted the way we think about bladder health. Counter to traditional thinking that healthy urine is sterile and should not contain any bacteria, Dr. Groah and her team have discovered that, in fact, the bladder contains a delicately balanced microbiome. In the bladder’s microbiome, a variety of bacteria maintain a homeostasis that varies within and across individuals.
-
Changes and imbalances in the microbiome are often characteristic of disease states, such as UTI in patients with spinal cord injuries who suffer from NLUTD. Dr. Groah’s research indicates that in these patients, certain beneficial bacterial strains, including but not limited to Lactobacillus rhamnosus, are depleted, while detrimental bacterial strains thrive.
-
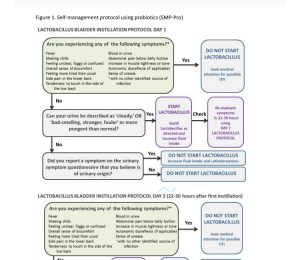
The screening, diagnosing, and treatment method invented by Dr. Groah and her team uses a questionnaire to track urinary symptoms in SCI patients at risk for UTI. For patients whose symptoms reach a certain threshold of risk for UTI, Lactobacillus rhamnosus GG, a probiotic bacteria, is inserted directly into the bladder to help rebalance the microbiome.
What is its current status?
Dr. Groah and her colleagues are currently conducting clinical trials, funded by a contract through the U.S. Department of Defense - Congressionally Directed Medical Research Programs, to test whether direct instillation of Lactobacillus rhamnosus GG into the bladder will alleviate or decrease UTI symptoms and the frequency of recurring UTIs.
Dr. Groah has completed a Phase I safety and tolerability study and is currently funded to begin two Phase II efficacy and dosing studies in patients with both indwelling and intermittent catheters.
MedStar Inventor Services has filed and has been issued a US Patent (US 9,962,416) based on Dr. Groah’s important work.
The MedStar Inventor Services team is now seeking a licensing/collaboration partner to develop and commercialize this technology. Please contact us at invent@medstar.net.
Figures
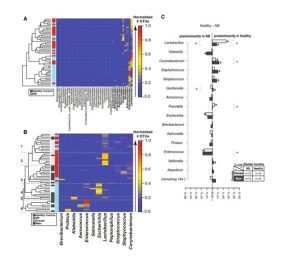
Differences in relative bacterial amounts between a neuropathic and healthy bladder in males and females: The bladder microbiome of patients with and without NLUTD was sequenced and compared. Patients with NLUTD have more of some bacteria and less of others when compared to healthy people. (Source: Fig. 1, J. Urol. 2016 Aug; 196(2):579-87. doi: 10.1016/j.juro.2016.01.088. Epub 2016 Jan 22.)
Phylogenetic diversity of Lactobacillales in human urine: Human urine not only contains many types of bacteria, but also great diversity within each species. This image shows the diversity of Lactobacillus in healthy individuals (dark blue), mostly healthy (light blue), only NLUTD (red), mostly NLUTD (pink/salmon). (Source: Fig. 4, J. Urol. 2016 Aug; 196(2):579-87. doi: 10.1016/j.juro.2016.01.088. Epub 2016 Jan 22.)
Self-management protocol: This figure illustrates the patient self-management protocol for direct instillation of probiotics.
Publications
-
Groah et al. (2016). Redefining Healthy Urine: A Cross-Sectional Exploratory Metagenomic Study of People With and Without Bladder Dysfunction. The Journal of urology, 196(2), 579–587.
https://pubmed.ncbi.nlm.nih.gov/26807926/ -
Forster et al. (2021). A single intravesical instillation of Lactobacillus rhamnosus GG is safe in children and adults with neuropathic bladder: A phase Ia clinical trial. The journal of spinal cord medicine, 44(1), 62–69.
https://pubmed.ncbi.nlm.nih.gov/31100050/
References
- Awad RA. Neurogenic bowel dysfunction in patients with spinal cord injury, myelomeningocele, multiple sclerosis and Parkinson’s disease. World Journal of Gastroenterology. 2011;17(46):5035. doi:10.3748/wjg.v17.i46.5035
- Dorsher PT, McIntosh PM. Neurogenic Bladder. Advances in Urology. 2012;2012:1-16. doi:10.1155/2012/816274
- Manack A, et al. Epidemiology and healthcare utilization of neurogenic bladder patients in a US claims database. Neurourology and Urodynamics. 2011;30(3):395-401. doi:10.1002/nau.2100
- Faaborg PM, et al. Autonomic dysreflexia during bowel evacuation procedures and bladder filling in subjects with spinal cord injury. Spinal Cord. 2014;52(6):494-498. doi:10.1038/sc.2014.45
- Groah SL, et al. Redefining Healthy Urine: A Cross-Sectional Exploratory Metagenomic Study of People With and Without Bladder Dysfunction. Journal Urol. 2016 Aug;196(2):579-87. doi: 10.1016/j.juro.2016.01.088. Epub 2016 Jan 22.