Background
Located in the heart of the nation’s capital, MedStar Washington Hospital Center is among the 100 largest hospitals in the nation, receiving more than 88,000 total Emergency Department (ED) visits in a year. As with many other urban EDs, overcrowding and complicated care can lead to long patient wait times.
In response, the hospital successfully implemented an in-person provider-in-triage (PIT) program. This essentially stationed a physician to assist patients right after they entered the ED from the waiting room. It reduced “door-to-doctor time,” the number of patients leaving the ED without being seen, and the wait time for medications. The PIT shift could be especially tough for the physician, however, who saw up to 90 patients and was stationed in a location prone to interruptions despite it being convenient for workflow.
In 2015, the MedStar Institute for Innovation (MI2) and MedStar Emergency Physicians recognized an opportunity to leverage telehealth advancements to evolve, modernize, and further enhance the already successful PIT program. They partnered with a startup company to consider how workflow improvements and telehealth technology could provide faster emergency care and improve both the patient and clinician experience. They piloted what eventually became the MedStar Health Emergency Department (ED) TeleTriage Program, starting at MedStar Washington Hospital Center.
Idea
Under the ED TeleTriage model, the physician who used to be stationed near the entrance of the ED for the PIT shift now works from a remote command center—yet remains central to the ED workflow. First, a triage nurse in the ED interviews the patient in-person. Then, the nurse connects to the off-site attending physician via a video connection and summarizes the patient’s symptoms to the physician with the patient present. Meanwhile, the physician in the remote command center looks at computer screens—one displaying a secure, live, two-way video and audio connection, and the other showing the electronic health record (EHR).
After listening to the triage nurse’s summary, reviewing the patient’s EHR, and interacting directly (but virtually) with the patient, the physician institutes a diagnostic and treatment plan with direct order entry. Instead of returning to the waiting room, the patient transitions to the internal area of the ED where labs are drawn, medications are given, and patients are transported to radiology.
This model eliminated some repetitive steps that used to require the patient to speak to the nurse and physician separately. Instead, while all patients still see a provider and receive the usual evaluation and management, this connected step improves efficiency and leads to shorter waits for the patient. Approximately one third of the time, the patient requires no additional diagnostic tests or medications than the ones ordered by the PIT physician, and the primary clinical team can finalize the patient’s ED visit based on the initial interventions.
Impact

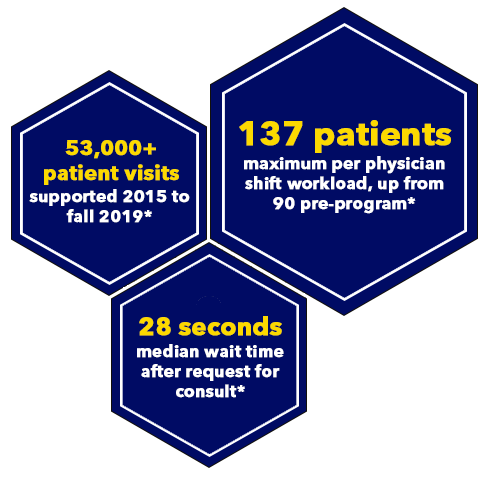
From 2015 to fall 2019, more than 50,000 patient visits had been recorded via the TeleTriage model. The median wait time between the nurse’s request for a consult and the time the physician sees the patient on the screen was 28 seconds.
Pre-TeleTriage, the maximum workload per PIT shift was 90 patients. Through the new model, that number rose to 137 patients—without using any additional physician resources. The environment is also vastly improved for the physicians: they can sit more, experience less interruptions, and can even use a treadmill desk.
This model has been successful at MedStar Washington Hospital Center and has been piloted in other MedStar Health hospitals and urgent care centers.
July 2021 Update
Since this story was first shared in October 2019, the TeleTriage program had continually expanded along with successful pilots, including smaller scale general teleconsults being offered from the bunker. Prior to the COVID-19 pandemic, the team was supporting additional MedStar Health emergency departments and urgent care sites, and even created and staffed a second “bunker” to further serve the system’s northern region and plan for additional growth.
In March 2020, the TeleTriage and teleconsult bunker infrastructure evolved and scaled to become instrumental in MedStar Health’s COVID-19 response. To help manage possible overcrowding and surging across the system, the MI2 MedStar Telehealth Innovation Center (MTIC) and MedStar Emergency Physicians (MEP) teams were charged to quickly make it possible for designated MedStar Health teams to call an emergency medicine provider in what became known as the MedStar Acute Care Coordinating Center (MAC3) during the pandemic.
The MAC3 was quickly supporting a wide range of locations:
-
MAC3 providers were accepting calls from inside all MedStar Health emergency departments, 24/7.
-
The team was also supporting tents outside emergency departments for the Evaluate, Treat, Disposition (ETD) workflow. This positioned in-person emergency department triage nursing staff to present well-appearing, low-risk patients with suspected COVID-19 infection to a provider in the MAC3 for evaluation, consideration of testing, and a disposition decision of discharge or initiating care for ongoing treatment in the emergency department.
-
Additionally, MTIC and MEP were charged with giving all MedStar Health urgent cares access to the same MAC3, growing the number of supported urgent care sites from five to 33 (the number following the Righttime Medical Care acquisition).
-
Similar infrastructure was established for locations at a smaller scale, including skilled nursing facilities, inpatient units, and MedStar Health Home Care.
In the first year of the pandemic response, MAC3 delivered an estimated 84,470+ telehealth sessions from March 13, 2020 to March 13, 2021. As of May 2021, MAC3 had supported more patient interactions than any one MedStar Health emergency department in the previous 12 months, and presently treats around 350-400 patient contacts a day. Clinical operational leadership of the MAC3 was also formalized given the scale of its service, supported by a medical director, lead physician assistant, and administrative support. The team even published some of its results in The Journal of Emergency Medicine study, titled “Preliminary Assessment of a Telehealth Approach to Evaluating, Treating, and Discharging Low-Acuity Patients With Suspected COVID-19.”
MTIC’s and MEP’s long-time aspirations to evolve and scale the TeleTriage program have been realized in MAC3, both in response to the COVID-19 pandemic and thanks to continued collaboration and innovation across the system. In the process, the MAC3 has made enormous contributions to patient care, provider well-being, quality and safety, and even financial stability. Looking ahead, this multi-faceted, system-wide service will continue to play a pivotal role in caring for the communities MedStar Health serves.
Resources
Websites
News
Press Coverage:
- Becker’s Hospital Review, "MedStar Health reduces certain ED visit lengths by nearly 63% via telehealth" (October 26, 2020)
- Bloomberg, “Automation Actually Creates More Jobs, at Least in the Beginning” (February 13, 2019)
-
NBC Washington, “Virtual ER Cuts Down on Wait Times at MedStar” (December 18, 2017)
-
Washington Business Journal, “How one D.C. Hospital cut Down its ER Wait Times, Some of the Longest in the City” (May 15, 2017)
Other Coverage:
-
MI2 Newsroom, “MedStar Health research highlights the benefits of integrating telehealth into the Emergency Department workflow during COVID-19” (October 26, 2020)
-
American Hospital Association, “Members in Action Case Study: TeleTriage Emergency Department Program, MedStar Washington Hospital Center, Washington, D.C.” (May 2018)
-
Advisory Board, “How a MedStar Hospital Slashed ED Wait Times by More Than 1 Hour” (May 22, 2017)
Publications
-
The Journal of Emergency Medicine, “Preliminary Assessment of a Telehealth Approach to Evaluating, Treating, and Discharging Low-Acuity Patients With Suspected COVID-19” (August 7, 2020)
Page last updated: 7/1/21
Page first published: 10/4/19
Summary
The team developed a virtual triage program for faster emergency care.Team
MedStar Telehealth Innovation CenterMedStar Emergency Physicians