Background
Sepsis is a spectrum of organ dysfunction that occurs when the body responds to infection. With more than a million people in the United States affected each year, sepsis cases account for billions of dollars in hospital costs. Despite an increasing number of cases—a quarter of which result in death—awareness of sepsis is low and many septic patients are not diagnosed at an early stage when aggressive treatment is most effective.
Currently, there are multiple scoring systems to quantify sepsis severity and the probability of various outcomes (e.g., mortality). Complex scoring systems that integrate organ failure assessment scores and general severity scores, which can be critical to sepsis detection and treatment, demonstrate opportunities to support clinical decision-making. However, these scoring systems are not generally incorporated into the electronic health record (EHR) which traditionally deploys binary diagnostic tools. In the absence of integrated alerts, clinicians have to "hunt and gather" in the EHR to identify sepsis and its progression by looking for related clues in the patient’s medical history, vital signs, and clinical lab values.
Given the current landscape, existing alerts have not been widely evaluated and assessed, leading to little consensus on how sepsis-related warnings should be generated and displayed to clinicians. In turn, time pressure, competing demands, and ambiguous alert design reduce clinicians’ opportunity to detect the signs of sepsis. Clinicians need improved EHR alerts as clinical decision support (CDS) tools at the point of care, affording rapid and accurate analysis and tailored treatment solutions in order to combat high mortality rates.
Idea
In 2016, MedStar Health National Center for Human Factors in Healthcare researchers, in partnership with the MedStar Health Research Institute, were awarded a prestigious, four-year Research Project Grant (R01) from the National Institutes of Health to develop a framework to optimize sepsis alert design.
The research focuses on developing and testing multiple enhanced visual display models that integrate patient data into validated sepsis staging scores. The ultimate goal of the research is to inform the development of future real-time CDS tools that optimize the organization, management, presentation, and utilization of information. Priorities therein include differentiating alerts, reducing alert fatigue, bridging the gap between novice and expert thinking, and creating a universal standard for sepsis alert design.
Impact
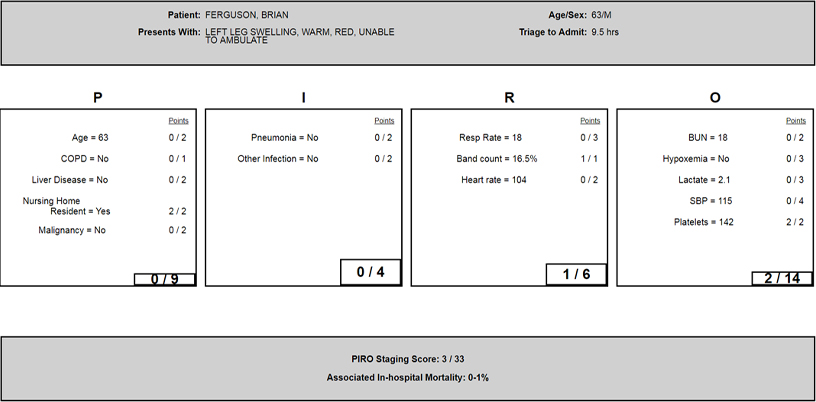
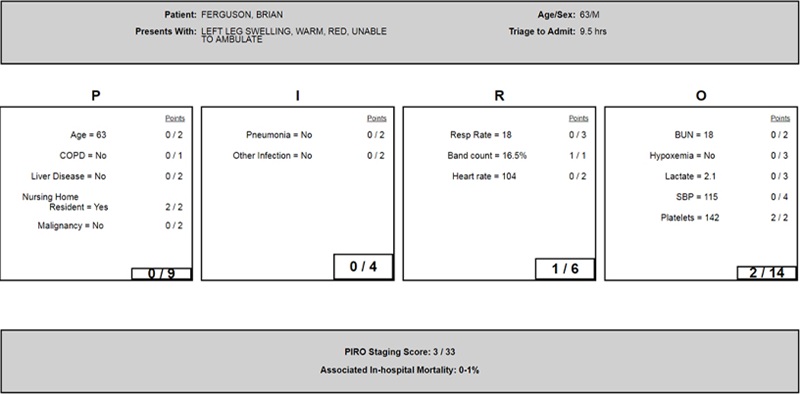
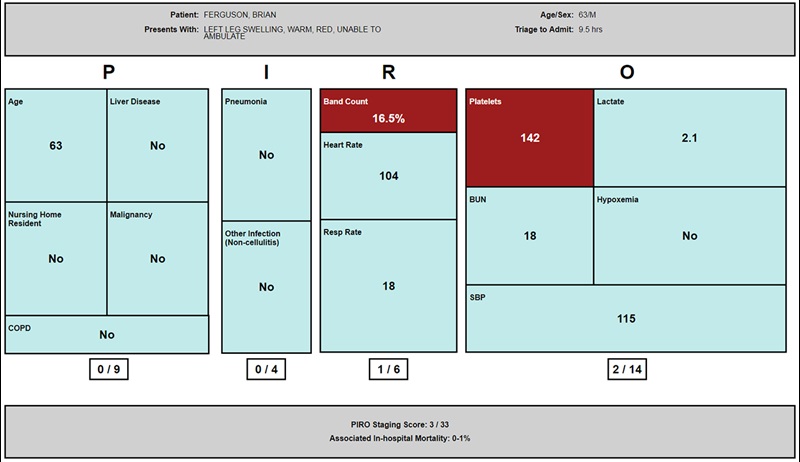
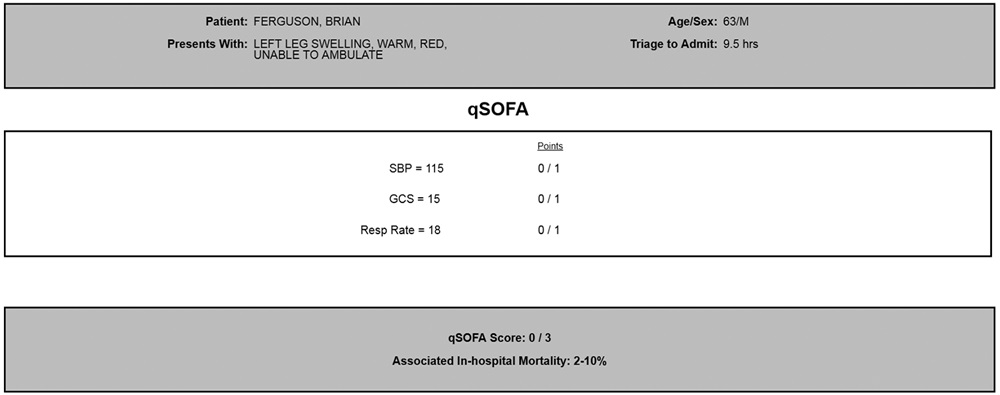
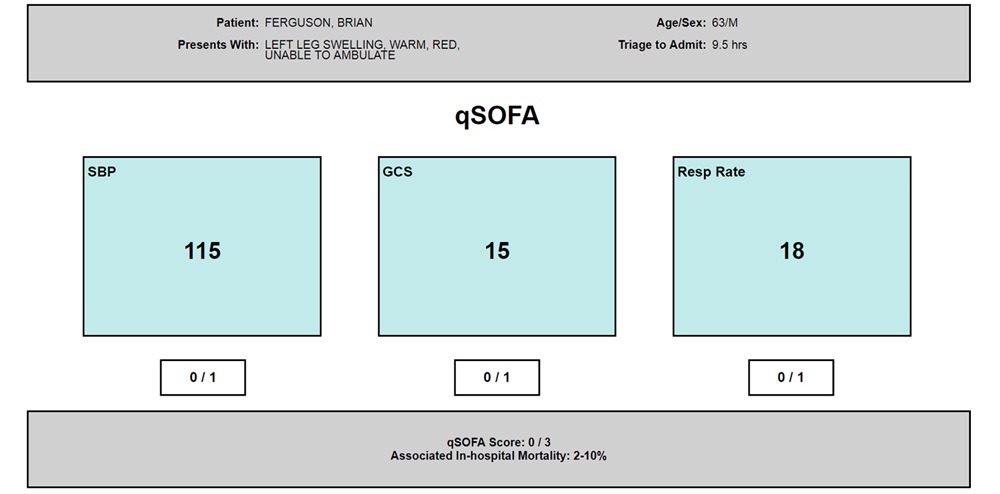
The study has resulted in the development of four sepsis alert designs (text and figure displays) based on two sepsis staging models: quick Sepsis-Related Organ Failure Assessment (qSOFA) and Predisposition, Infection, Response, Organ Failure (PIRO).
Using a simulated EHR environment, nurses and physicians were asked to examine test patient records, review a provided alert, and evaluate clinical information. Outcomes reported included objective and subjective measures of preference and performance. Using eye-tracking software and interview methods, the study assessed the impact on provider action and performance by varying: (1) how clinical information is displayed (e.g., text, figure display), (2) the amount of content provided in the alert, and (3) the sepsis severity (e.g., low, high) of the test patient records.
The study also utilized the ShadowBox Process, which allows novices to “see the world through the eyes of the experts” without the experts being present. The results of the study will help identify gaps in novice understanding, aid in the evolution of novice to expert thinking, and identify potential improvements in the clinical decision-making process.
The ultimate goal of this research is to develop an evidence-based framework to optimize clinical decision support in the EHR. As demands on healthcare providers increase, the potential for safety-critical interaction problems with the EHR also increases. The results of our research will enable design changes in the EHR to improve the usefulness of sepsis alerts and reduce unintended consequences associated with current alert management.
Images
July 2021 Update
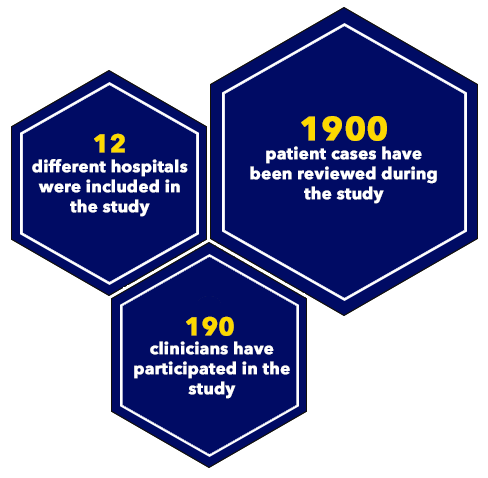
The research team completed usability testing with 190 clinicians across 12 different hospitals and is currently analyzing results on clinician preference, performance, and usability of the different enhanced visual displays.
Preliminary research findings suggest:
- Providers prefer clinical decision support (CDS) that offers: (1) more comprehensive models with more clinical information over simple models with less information; (2) enhanced visual displays over basic text design.
- Enhanced visual display CDS alerts providers to information they otherwise may have missed, including information about comorbidities, organ dysfunction, and risk of in-hospital mortality.
- Enhanced visual display models scored better with regards to subjective usability, while simpler models scored better objectively using the System Usability Scale. This indicates more complex models outperform simpler ones but have a steeper learning curve.
Additionally, in response to the COVID-19 pandemic, the research team received a grant award supplement from the National Institutes of Health (NIH) to evaluate CDS for diagnosis and clinical management of the disease. The project evaluates technical and design features for tools that identify the presence of COVID-19 in the variety of ways in which it presents, the availability of data elements, the accuracy of diagnostic tests, and the disease’s highly infective nature.
Resources
Websites
News
-
MedStar Institute for Innovation News Feed: “Texas A&M School of Public Health: Miller Awarded 1.4 million to Develop Sepsis Alert System”
-
Becker’s Health IT & CIO Report: “5 Tips for Developing EHR Alerts”
Publications
Key Publication:
-
Health Informatics Journal, “Informatics and Interaction: Applying Human Factors Principles to Optimize the Design of Clinical Decision Support for Sepsis”
Additional Publications:
-
International Journal of Medical Informatics, “The Design of Decisions: Matching Clinical Decision Support Recommendations to Nielsen’s Design Heuristics”
-
Critical Care Nursing, “Evaluation of User Interface Alert Displays for Sepsis Clinical Decision Support”
-
Journal of Critical Care, “Not all Organ Dysfunctions are Created Equal - Prevalence and Mortality in Sepsis”
-
American Journal of Hospital Medicine, “Translating Prediction to Decision: A Framework to Tackle Risk Identification and Presentation Challenges in Sepsis”
-
Journal of the American Medical Informatics Association, “Interface, Information, Interaction: A Narrative Review of Design and Functional Requirements for Clinical Decision Support”
Please note: Images on this page contain fictitious patient data or are otherwise altered for confidentiality.
The overview above reflects work completed while the MedStar Health National Center for Human Factors in Healthcare was part of the MedStar Institute for Innovation. In July 2020, the Human Factors Center transitioned to its new organizational home, MedStar Health Research Institute, and still remains a key collaborator of MI2. Visit the Human Factors Center website for the latest information on its work.
Page last updated: 7/1/21
Page first published: 10/10/19
Summary
The team is informing the development of real-time clinical decision support tools to detect and treat sepsis.
Team
MedStar Health National Center for Human Factors in Healthcare
Status
Active